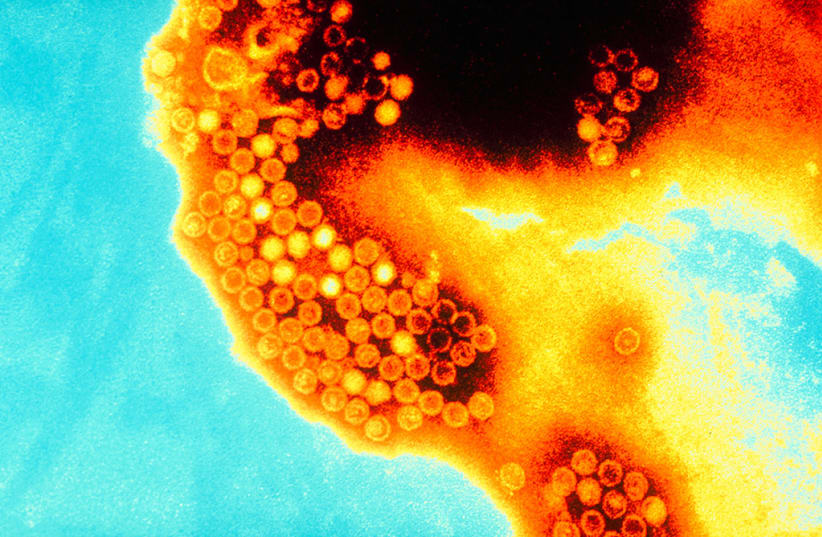
Long COVID may be the cause of unexplained cases of hepatitis in children around the world in recent months, Israeli researchers from Schneider Children’s Medical Center, Rabin Medical Center – Beilinson Hospital, Rambam Medical Center and Tel Aviv University found in a study recently published in the peer-reviewed Journal of Pediatric Gastroenterology and Nutrition.
12 cases of unexplained acute hepatitis in children have been reported so far in Israel.
The Israeli scientists who conducted the study noted that liver injury has been recorded in adult patients with severe coronavirus infections and that children can be affected with multisystem inflammatory syndrome (MIS-C) as a result of COVID-19, which can injure the liver. Post-COVID-19 liver injuries have been increasingly reported among adults as well.
The new Israeli study analyzed the cases of five patients who were hospitalized in Schneider Children's Medical Center last year due to liver injury. All five patients had tested positive for SARS-CoV-2 before presentation of symptoms.
The first patient, a 3-month-old infant, was hospitalized for acute liver failure 21 days after being diagnosed with COVID-19. 11 days later, he underwent a liver transplant. The infant was negative for adenovirus, SARS-CoV-2, Epstein-Barr virus, cytomegalovirus (CMV) and herpes simplex virus.
The second patient, a 5-month-old patient, was hospitalized with a fever, jaundice and an enlarged liver (hepatomegaly) and his condition deteriorated, leading to him needing a liver transplant. He tested positive for both adenovirus and SARS-CoV-2. After the transplant, he tested positive for CMV as well.
The third patient, a previously healthy 8-year-old boy, tested positive for the novel coronavirus before experiencing liver injury. About 130 days after his COVID-19 diagnosis, he arrived at the hospital with abdominal pain, vomiting and jaundice. He was not found to be infected with adenovirus.
The fourth patient, an 8-year-old boy, began experiencing abdominal pain, vomiting, diarrhea and jaundice about 90 days after being diagnosed with COVID-19. He was not found to be infected with adenovirus.
The fifth patient, a previously healthy 13-year-old boy, tested positive for SARS-CoV-2 after presenting with weakness, diarrhea, jaundice and abdominal pain. 53 days after testing positive, he arrived at the hospital with vomiting, abdominal pain, jaundice, hepatomegaly and liver injury. During his hospitalization, he needed to undergo a liver transplant. After the operation, he tested positive for CMV and adenovirus.
The study noted that the two 8-year-olds and the 13-year-old experienced acute hepatitis with cholestasis (decreased bile flow), while the two infant patients experienced acute liver failure.
The patients analyzed by the study had asymptomatic or mild presentation of COVID-19 before the onset of liver issues, while among adults most patients who experienced liver issues had been in the ICU for a prolonged period while suffering from severe cases of COVID-19.
Other studies conducted around the world have also found that some COVID-19 patients suffer from liver issues weeks or even months after being diagnosed with COVID-19.
The scientists noted that while many of the unexplained acute hepatitis cases around the world have also tested positive for adenovirus, this may not be the cause for the liver issues as adenovirus usually causes severe hepatitis in immunocompromised patients and these patients were healthy before experiencing hepatitis.
The scientists analyzed samples of the livers of the patients to see if there were signs that adenovirus had caused the damage to the organ, but did not find any antigens indicating adenoviruses nor any features suggesting hepatitis caused by an adenovirus. A number of other analyses of the liver tissue of other cases from around the world also failed to find any signs of liver damage caused by an adenovirus.
A number of possible mechanisms may cause liver injury during acute disease and after recovery from COVID-19, including direct viral damage, injuries caused by an aberrant immune response, restricted blood flow (ischemia), increased blood clotting (hypercoagulability state) and drug-induced injuries.
As none of the patients in the study had severe cases of COVID-19, the scientists stated that this suggested that the liver injury may have been caused by direct viral damage caused through the ACE2 receptor to which the SARS-CoV-2 binds and enters the cell.
Another possible mechanism that could have caused the liver damage is if the immune system either underreacted or overreacted to the infection. Autoimmune and auto-inflammatory diseases such as MIS-C have been reported in both children and young adults with long COVID-19, which could lead to liver disease.
Inflammation and an unusual immune response could also have impaired the health of the patients and led to disease in predisposed individuals. The second patient in the study had a systemic inflammatory syndrome called secondary hemophagocytic lymphohistiocytosis (HLH), which could support the theory that the liver injury was caused by an immune-mediated mechanism.
The scientists concluded that the most likely causes of the acute hepatitis were either a post-infection immune reaction like MIS-C or an abnormal immune response to the novel coronavirus which primed the body for other infectious agents like adenovirus.
Global health community continues to investigate
In early April, the United Kingdom reported an increase in acute hepatitis cases with an unexplained cause among previously healthy children.
Since then, about 700 probable cases of unexplained acute hepatitis have been reported from 34 countries, according to the World Hepatitis Alliance. The World Health Organization (WHO) assesses the global risk from the unexplained hepatitis cases as moderate.
Of the cases, at least 38 have required transplants and ten have died. Since the cases were first reported, the WHO and US Centers for Disease Control and Prevention (CDC) have posited that an adenovirus may be the cause, as some of the affected patients were also found to be infected with an adenovirus. In England, 68% of cases tested positive for adenovirus.
"It’s the first time so many cases of severe acute hepatitis have been seen."
Dr. Philippa Easterbrook, technical lead of the incident team at WHO headquarters
"In terms of how worried we should be about this outbreak, it’s the first time so many cases of severe acute hepatitis have been seen," said Dr. Philippa Easterbrook, technical lead of the incident team at WHO headquarters, at the World Hepatitis Summit last week. “A proportion of cases have developed liver failure, required transplantation or resulted in death. It has to be taken seriously. An important step at the moment is to understand its cause.”
The UK Health Security Agency (UKHSA) is set to publish the preliminary findings of a epidemiological study into the acute hepatitis cases on June 16.
A pre-print study by researchers from KU Leuven found nine cases of unexplained acute hepatitis from September 2021 to April 2022, when high levels of both adenovirus and SARS-CoV-2 were circulating among the general population in Belgium. No cases of unexplained acute hepatitis were found in earlier timeframes checked by the researchers.
The researchers from KU Leuven stressed that their observations "do not confirm or exclude the possibility that adenovirus or SARS-CoV-2 infections are contributors to the rise in acute hepatitis cases in children." They added that if either or both viruses do contribute, then their findings show that only a small minority of infections are likely to lead to severe hepatitis, as there were only a few hospitalizations due to hepatitis while there was a high rate of community transmission of both viruses.